Pain Reprocessing & Neuroplastic Pain Therapy in Seattle and Portland
Individual pain therapy grounded in contemporary pain science and neuroscience-based approaches, including Pain Reprocessing Therapy (PRT). Offered remotely to adults throughout Washington and Oregon.
When Doing Everything Right Still Hasn’t Helped
Living with chronic pain often means living with uncertainty — about your body, your future, and whether anyone truly understands what you’re experiencing.
Many people arrive here after years of trying to do everything “right”: medical workups, physical treatments, mindset shifts, pacing strategies — only to be left with pain that continues without a clear explanation. Others have been told their pain is stress-related or psychological without being given a framework that actually makes sense or leads to change.
I understand how invalidating that can feel.
I also bring lived experience with chronic pain to this work. While that experience is not the focus of our sessions, it informs how I approach pacing, autonomy, and trust. I know the difference between being asked to push through and being supported in a way that respects how real pain actually works.
This work is for people who want an explanation that is neither dismissive nor purely structural — and who are open to understanding pain as a nervous system process that is real, meaningful, and changeable.
What If There Was Another Way?
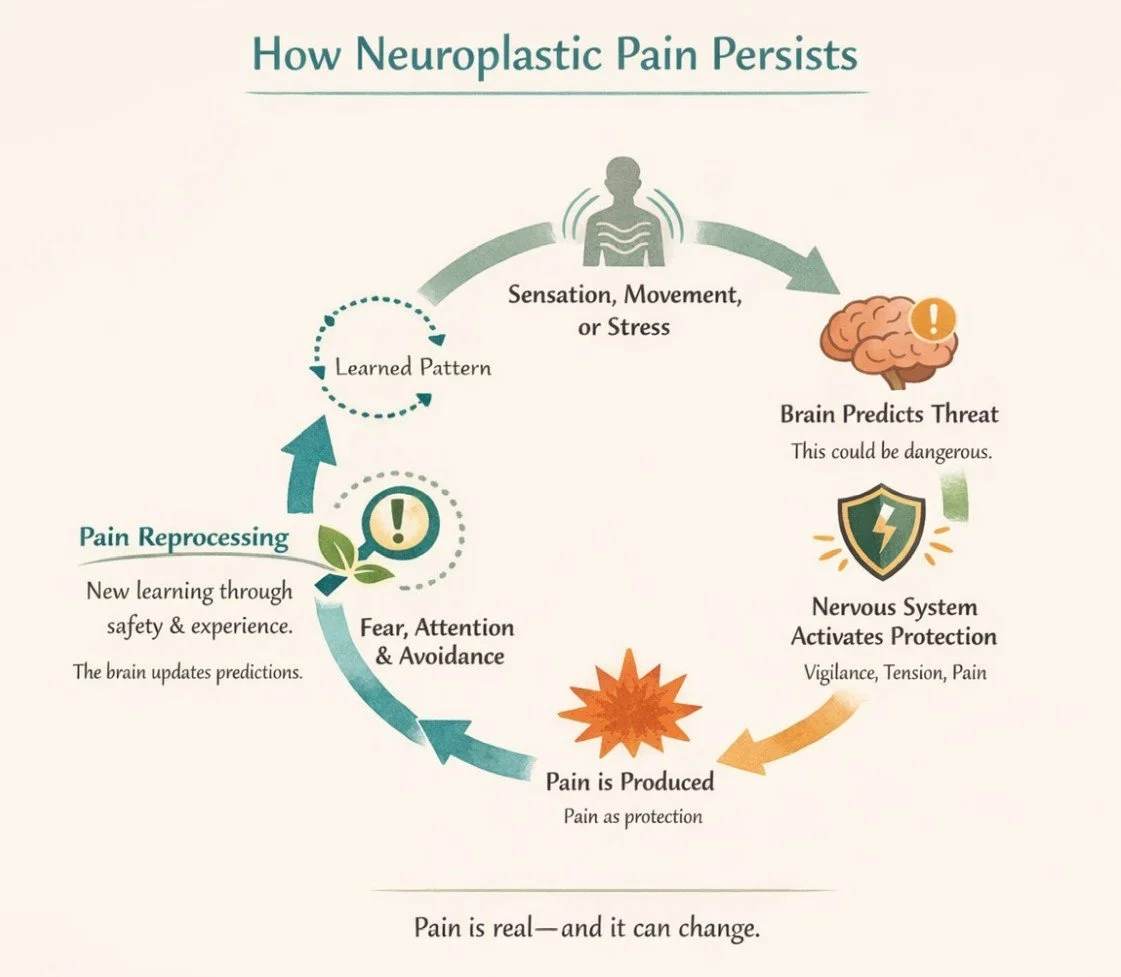
When you touch a hot stove, pain shows up quickly because your brain believes there is danger and wants you to move away. But the brain can also produce pain even when there is no ongoing injury — especially if it has learned to expect threat.
This is what often happens in chronic pain.
Over time, the nervous system can become overprotective. It stays on high alert, continuing to send pain signals long after tissues have healed, or in situations that are not actually dangerous. This doesn’t mean the pain is imagined or psychological. It means the system learned a pattern that no longer matches what’s happening in the body.
Pain is not a direct measure of damage in the body. It is a protective signal created by the nervous system to keep you safe.
This type of pain is often called neuroplastic pain — pain that is real, learned, and changeable.
Pain is influenced by many factors, including:
past injury or illness
stress and emotional load
fear, attention, and expectation
meaning, context, and past experiences
None of these factors “cause” pain on their own. But together, they shape how the nervous system decides whether something is dangerous enough to hurt.
This work focuses on helping the nervous system update those danger signals — not by forcing symptoms away, but by teaching the brain, through experience, that it no longer needs to protect in the same way.
When the brain learns that it is safe again, pain often begins to change.
But Will This Approach Help Me?
People often arrive here searching for help with a specific diagnosis — such as back pain, migraines, fibromyalgia, pelvic pain, tinnitus, or IBS. While these conditions can look very different on the surface, what matters more than the diagnosis is the pattern your symptoms follow.
This approach is often helpful when symptoms:
have lasted longer than expected
persist despite treatment or “normal” testing
spread, fluctuate, or change over time
feel worse with stress, fear, or certain situations
In these cases, symptoms are often being maintained by an overprotective nervous system rather than ongoing injury — which means they may be changeable, even if they’ve been present for a long time.
If you’re curious whether your symptoms fit this pattern, you may find it helpful to review the FIT criteria, a set of questions designed to help identify whether pain is likely being driven by nervous system sensitization rather than tissue damage.
This is not a diagnostic test or something you have to “pass.” It’s simply a way to notice patterns that often respond well to pain reprocessing and nervous-system-based work.
How Sessions Are Structured
Sessions follow a clear framework grounded in pain neuroscience and nervous system learning. The approaches below are integrated thoughtfully based on what best will support your safety and change. You don’t need to understand or “do” all of these for the work to be effective. Sessions will typically include one or more aspects of the following:
-
Pain Reprocessing Therapy forms the foundation of this work.
PRT is based on the idea that pain is often generated by the nervous system when it believes there is danger — even if there is no ongoing injury or damage in the body. Over time, the brain can learn to associate certain sensations, movements, or situations with threat, and pain becomes the signal it uses to protect you.
This doesn’t mean the pain is imagined. It means the nervous system has learned a pattern that hasn’t yet updated.
PRT focuses on helping the brain recognize when pain is being driven by learned threat rather than current danger. This happens through a combination of understanding why pain is happening and having real, in-the-moment experiences that allow the nervous system to learn something new.
In sessions, this may include:
learning how your nervous system produces and maintains pain
noticing patterns that suggest a sensitized or overprotective system
gently practicing ways of responding to sensations that reduce fear and threat
PRT is not about pushing through pain, ignoring your body, or forcing positive thinking. It’s about helping the nervous system experience — in a safe and gradual way — that it no longer needs to protect in the same way it once did.
As the brain updates its expectations, pain often begins to change.
-
For many people with chronic pain, the nervous system isn’t just responding to physical sensations — it’s responding to long-standing emotional patterns that have never felt safe to express.
This often shows up as:
chronic people-pleasing
difficulty setting boundaries
guilt when saying no or prioritizing yourself
fear of conflict or disappointing others
anger that gets pushed down or turned inward
shame about having needs, limits, or strong feelings
When emotions like anger, sadness, or assertiveness don’t feel safe, the nervous system stays on high alert. Over time, pain can become one of the ways that unexpressed stress and internal pressure show up in the body.
EAET-informed work helps bring awareness to these patterns — not to blame emotions for pain, but to reduce the internal threat that keeps the nervous system activated.
In sessions, this may involve:
noticing where you habitually override your own needs
understanding how guilt, shame, or fear of conflict affect your body
safely exploring emotions that have been avoided or suppressed
practicing more direct, honest internal and external expression
This is not about venting, rehashing the past, or forcing emotional release. It’s about helping your nervous system experience that expressing yourself — internally or externally — does not actually lead to danger.
As emotional flexibility increases, the nervous system often no longer needs pain as a protective signal in the same way.
-
Many people with chronic pain feel stuck in an internal tug-of-war.
One part of you may be driven to push through, stay productive, and “figure this out.” Another part may feel overwhelmed, shut down, or afraid of making things worse. You might notice harsh self-talk, pressure to perform, or a sense that you’re constantly managing yourself just to get through the day.
Parts-based work helps make sense of these inner dynamics without treating them as problems.
Instead of asking, “What’s wrong with me?” this approach asks, “What is each part of me trying to protect?”
From a pain perspective, these internal conflicts matter because ongoing self-pressure, vigilance, or self-criticism can keep the nervous system in a state of threat — even when there is no external danger.
In sessions, this may involve:
noticing the different internal voices or reactions that show up around pain
understanding how self-pressure, fear, or hyper-responsibility affect the body
reducing internal battles that keep the nervous system on high alert
building a more supportive internal relationship with pain and symptoms
This work is not about dissecting your personality or digging into childhood unless it’s relevant. It’s about helping the nervous system experience less internal friction, so it no longer needs to use pain as a signal to slow things down or demand attention.
Frequently Asked Questions (FAQ)
-
I can’t promise that — and anyone who does isn’t being honest.
What this work offers is a way to understand why pain is happening and to create the conditions where pain can change. For many people, pain reduces significantly or resolves as the nervous system learns that it no longer needs to protect in the same way. For others, pain becomes less intense, less frequent, or less consuming.
The focus here isn’t on guarantees or quick fixes. It’s on meaningful, lasting change based on how pain actually works — not just learning to tolerate it better.
-
Sometimes — but not always.
Many people have both structural contributors and nervous system sensitization. This work can be helpful when pain:
lasts longer than expected after healing
spreads or fluctuates
feels out of proportion to current tissue findings
If pain is primarily driven by active disease, ongoing injury, or structural instability, this approach may not be appropriate on its own. Part of the work is carefully assessing whether nervous system processes appear to be meaningfully involved.
This isn’t about ignoring structure — it’s about understanding when structure alone doesn’t explain what’s happening anymore.
-
CBT and behavioral pain management tend to focus on coping with pain: pacing, thought patterns, behavior changes, and learning how to live around symptoms.
Pain reprocessing and nervous system–based approaches aim at something different. Rather than managing pain long-term, the goal is to change the pain signal itself when pain is being generated by learned threat in the nervous system.
This work is less about “thinking differently” and more about helping the brain and nervous system learn something new through experience. For people whose pain hasn’t responded to coping-based approaches, that distinction matters.
-
There isn’t a single timeline.
Some people notice shifts relatively quickly once the nervous system begins to update. Others need more time, especially if pain has been present for many years or has become intertwined with long-standing patterns of stress, fear, or self-protection.
Progress isn’t linear, and it’s not something you can force. This work is usually time-limited and purpose-driven rather than open-ended, but readiness and nervous system safety matter more than speed.
-
This work is often a good fit if:
your pain hasn’t made full sense structurally
you’ve tried many approaches without lasting change
symptoms shift with stress, attention, or context
you’re open to understanding pain differently
It may not be a good fit if you’re looking for reassurance, passive treatment, or a step-by-step formula. Curiosity, openness, and willingness to engage matter more than optimism.
If you’re unsure, that’s okay. Fit is usually clarified through careful history and conversation, not a single checklist or diagnosis.
-
This isn’t a homework-heavy approach, and it’s not about tracking everything or doing exercises perfectly.
Between sessions, the work often looks like:
noticing patterns in pain, fear, or self-protection
experimenting gently with new ways of responding to sensations
applying insights from sessions in real-life moments
The goal isn’t to work harder — it’s to support nervous system learning through lived experience, at a pace that feels sustainable rather than overwhelming.
-
I work with people experiencing a wide range of chronic pain and persistent physical symptoms, including back and joint pain, migraines, fibromyalgia, pelvic pain, tinnitus, and irritable bowel symptoms (IBS).
What matters most isn’t the diagnosis, but the pattern — particularly whether symptoms appear to be maintained by an overprotective nervous system rather than ongoing injury alone. People with very different labels can benefit from the same underlying work when those patterns are present.
-
While this work is often associated with chronic pain, the same nervous system processes that generate pain can also contribute to other persistent physical symptoms.
Symptoms like tinnitus, irritable bowel symptoms (IBS), dizziness, or ongoing bodily discomfort can sometimes be maintained by an overprotective nervous system — especially when medical testing hasn’t fully explained their persistence or severity, and symptoms fluctuate with stress, attention, or context.
This work focuses on understanding whether symptoms appear to be driven by learned threat and sensitization rather than ongoing tissue damage or disease alone. When that pattern is present, nervous system–based approaches may be helpful — even when pain isn’t the primary complaint.
That said, not all non-pain symptoms are neuroplastic, and this approach isn’t a fit for everyone. Determining whether it makes sense in your case is part of the process and doesn’t require certainty upfront.

Neuroplastic healing can help you gain a deeper understanding of your pain experience on a holistic level, giving you the power to become an active participant in your own healing process and move towards a more pain-free life.
You don’t have to have everything figured out, or know whether this is “the thing” yet. If parts of this page felt familiar or quietly relieving, that’s often enough to start a conversation.